Table of Contents
To evaluate whether Maori benefit from specific funding we have to compare Maori health and life expectancy in the 1960s, when the Waitangi Tribunal was established, with recent Maori health outcomes and longevity after 45 years investment.
In the 1960s there was a genuine need for improvement. Compared to other ethnic groups Maori were sicker, had a shorter life expectancy, were poorer, over represented in welfare and prison, had higher rates of domestic abuse and more Maori children lived in poverty with higher child abuse and murder rates.
In a 1960 study the maori mortality rate was still about twice that of non-maori, with the greatest gap seen in the years of infancy and childhood.
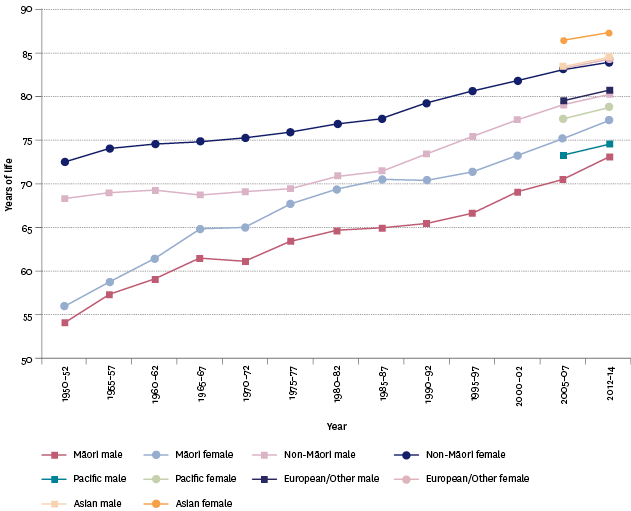
There are marked differences in life expectancy at birth between ethnic groups. In 2012–2014, non-Maori female life expectancy at birth was 83.9 years and non-Maori males 80.3 years, both being higher than Maori females’ and Maori males’ life expectancy at birth of 77.1 years and 73.0 years respectively. This difference reflects that Maori death rates are higher than non-Maori at nearly all ages, and this has to do with a number of factors including smoking rates and socio-economic factors.
The most recent data available is six years old! Given that we continue to invest in and expect better Maori health outcomes, why isn’t up to date data available?
[In the 1960s] Maori were affected more than non-Maori by degenerative conditions such as diabetes, cancer, heart disease and stroke, which had not been much in evidence before.
Maori health outcomes are presumed to lag behind other ethnicities. $56M was given to Maori who were predicted to be at higher risk of COVID because of a higher rate of pre-existing conditions like chronic lung disease (including cystic fibrosis, bronchiectasis, chronic obstructive respiratory disease and emphysema), severe asthma, serious heart conditions, hypertension, diabetes and chronic kidney and liver disease.
“As Maori academics, researchers and health professionals, we are extremely concerned about the impacts of the COVID-19 pandemic on our whanau and communities.
We are also worried by the inadequate focus on Maori health equity in pandemic planning within the health and disability system, and in the whole-of-government ‘one-size-fits-all’ approach.”
We have not had a “one size fits all” approach to Maori for decades. To pretend otherwise disguises the fact that the government is not reporting on Maori health outcomes despite providing additional funding. How do we know the money was well spent?
“The Government will spend more than $56 million on a specific Maori response action plan. The cross-sector announcement comes after growing criticism from the Maori community, iwi leaders and health experts.
Associate Health and Whanau Ora Minister Peeni Henare said the government’s $12.1 billion economic package and $500m health fund includes Maori families, workers and businesses but a separate plan was needed because Maori have specific challenges.
“We know that we need to help our people and provide targeted support to MAori businesses and help our vulnerable Maori communities.”
What are the specific challenges? Has anyone asked how the money was spent? Now that COVID has run its course in community transmission, did Maori contract more COVID, did more Maori die from COVID?
Either the $56M was money well extremely well spent or Maori are no more vulnerable than anyone else because Maori infections rates in Auckland were 0.2% compared to Other (non-Maori) at 0.5%. Maori had less COVID transmission than non-Maori. Could Maori integration with other ethnicities result in less, rather than more, vulnerability to new diseases than in the 1960s?
Out of the 22 people who died from COVID-19 how many were Maori? Why hasn’t the government made available the ethnic breakdown of deaths from COVID-19, given $56M was specifically alloted?
We won’t know the answer, because the answer does not fit the political narrative of the Waitangi Tribunal, who are fighting hard for more dollars for Maori, not less.
It is not hard to collect ethnic data on health outcomes, and given the amount of money spent specifically on Maori health, reporting should be mandatory.
Have Maori followed the same trend in COVID mortality as they did in infection rates, which is less than other ethnicities? It would be embarrasing for the government to admit the $56M Maori allocation for COVID was completely unnecessary!
If you enjoyed this BFD article please consider sharing it with your friends.