Table of Contents
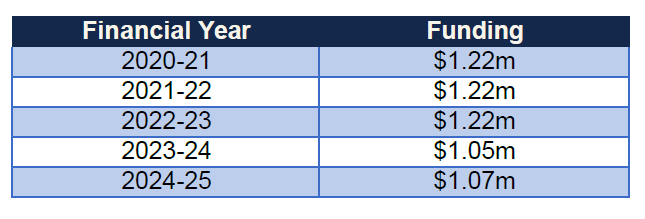
According to an Official Information Act response from Health NZ/Te Whatu Ora, the taxpayer is funding more than one million dollars each year towards enabling people to surgically change their sex via vaginoplasty, metoidioplasty and phalloplasty procedures. The demand is higher for the removal of the penis, testicles and scrotum. Demand for these surgical procedures is predominantly in the 18–25 and 26–35 age brackets.
According to Te Whatu Ora, “Of the 326 patients on the waiting list, 243 have requested a feminising procedure and 83 a masculinising procedure. Therefore, it can be assumed of the sex assigned at birth of these patients 243 were assigned male at birth and 83 assigned female at birth.” (our emphasis added)
Age ranges of the 326 patients are:
18–25 94
26–35 148
36–45 51
46–55 22
>55 11
Vaginoplasty involves removing the healthy penis, testicles and scrotum to create a vulva and vagina.
Metoidioplasty involves creating a penis about four to six centimeters long using the clitoris, which may be enlarged by hormone therapy. The surgery can be completed in stages, each performed a few months apart, depending on the patient’s objectives.
Phalloplasty uses a tissue flap from the arm or thigh to create a larger phallus that can accommodate a penile prosthesis and penetration. Phalloplasty is a multistage operation, with urethroplasty to enable standing urination performed later. Phalloplasty is complex and has a higher risk of complications, including infection, scarring, and narrowed urethra.
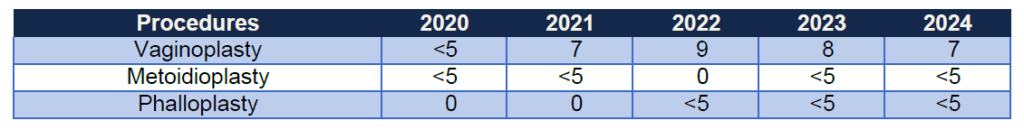
Despite the relatively small number of surgeries actually performed, the cost is significant.
[Where the number of individuals is less than five, Health New Zealand used <5 to avoid revealing sensitive information about potentially identifiable individuals in the data. It is also important to note that some patients may require more than one procedure.]
Health NZ were unable to quantify the costs of mental health assessment, psychiatric support or counselling – if these even occurred.
A Swedish study followed a transgender group of adults from 1973-2003. This study found:
Persons with transsexualism, after sex reassignment, have considerably higher risks for mortality, suicidal behaviour, and psychiatric morbidity than the general population. Our findings suggest that sex reassignment, although alleviating gender dysphoria, may not suffice as treatment for transsexualism, and should inspire improved psychiatric and somatic care [restore the natural balance within the body-mind system to resolve physical and mental stress) after sex reassignment for this patient group.
And a recent Finnish study said:
Although the rate of suicide [in the Finnish study] is just over four times higher among trans young people than their peers, this is explained by their more serious psychiatric problems. When these psychiatric problems are taken into account, there is no evidence that transgender people have a higher rate of suicide.
This Finnish study vindicates their decision four years ago to adopt a more cautious treatment policy which first targets psychiatric, social and educational problems among gender-distressed youth before any assumption of a stable trans identity justifying ‘experimental’ affirmation with hormones or surgery.
The researchers say in their BMJ Mental Health paper:
It is of utmost importance to identify and appropriately treat mental disorders in adolescents experiencing gender dysphoria to prevent suicide; in addition, health policies need to ensure that accurate information is provided to professionals along these lines.
A study published in April entitled “Risk of Suicide and Self-Harm Following Gender-Affirmation Surgery” evaluated patient data from nearly 60 US healthcare organisations, comprising millions of patients. The study concluded:
Individuals who underwent gender-affirming surgery had a 12.12-fold higher suicide attempt risk than those who did not.
Those who had undergone gender-transition surgeries were nearly five times more likely to attempt suicide than those who had undergone tubal ligations or vasectomies, the study found. It warned:
Gender-affirming surgery is significantly associated with elevated suicide attempt risks, underlining the necessity for comprehensive post-procedure psychiatric support.
What is most concerning is that the demand for these unnecessary operations here in New Zealand is only likely to increase.
According to Official Information Act data gained by Family First from the Department of Internal Affairs, almost 900 people in total have changed their birth certificates to their ‘self-identified gender’ since the new birth certificate law came into force last year. Children are changing the sex on their birth certificate, including 47 children 15 years or younger.
Demand to be recognised as a female was greatest with 445, followed by male 302, and non-binary 142.
Health NZ say that since 2020 the service has been publicly funded to deliver up to 14 gender-affirming genital surgeries (either feminising or masculinising) per year.
In a poll at the end of 2018, 63 per cent opposed taxpayer funding for hormone treatment and surgery for people who wished to change their sex. Twenty-seven per cent supported it and a further 11 per cent were unsure or refused to say.
This article was originally published by Family First New Zealand.