Table of Contents
Maryanne Demasi
Maryanne Demasi, 2023 Brownstone Fellow, is an investigative medical reporter with a PhD in rheumatology, who writes for online media and top tiered medical journals. For over a decade, she produced TV documentaries for the Australian Broadcasting Corporation (ABC) and has worked as a speechwriter and political advisor for the South Australian Science Minister.
In January 2021, in the absence of any human data in pregnancy, the CDC stated on its website that mRNA vaccines were “unlikely to pose a specific risk for people who are pregnant.”
Former CDC director Rochelle Walensky backed it up with a full-throated endorsement of COVID-19 vaccination in pregnancy.
“There is no bad time to get vaccinated,” said Walensky.
“Get vaccinated while you’re thinking about having a baby, while you’re pregnant with your baby or after you’ve delivered your baby,” she added.
Behind the scenes, however, Pfizer was scrambling to conduct a clinical trial of its vaccine in pregnant women.
By February 2022, Pfizer revealed it still did “not yet have a complete data set.” Its statement read:
“The environment changed during 2021 and by September 2021, COVID-19 vaccines were recommended by applicable recommending bodies (e.g., ACIP in the U.S.) for pregnant women in all participating/planned countries, and as a result the enrollment rate declined significantly.”
This month, Pfizer finally posted some trial results on clinicaltrials.gov.
The data do not appear in a peer-reviewed journal or a pre-print, nor has it been submitted to the FDA for evaluation.
I spoke with experts who have analysed the data with a fine-toothed comb and made some alarming observations.
Trial design
Pfizer originally planned to recruit 4,000 healthy women aged 18 or older who were 24 to 34 weeks pregnant. Half would be randomised to the vaccine and the other half to a saline placebo.
The efficacy and safety of the vaccine would be determined by assessing COVID-19 cases, antibody responses, and adverse events.
Peculiarly, Pfizer planned to vaccinate all the mothers in the placebo group, one month after giving birth to their babies.
Retsef Levi, a professor at the Massachusetts Institute of Technology Sloan School of Management said that vaccinating mothers in the placebo group during the assessment period would introduce a new variable into the experiment and “corrupt” the data.
“We now know that mRNA from the vaccine is detected in the breast milk, so those babies born from mothers who were all vaccinated after giving birth, are also potentially exposed to mRNA through breastfeeding,” explained Levi.
“This corrupts the comparison of the two groups of babies because you don’t have a true control group anymore,” he added.
Sample size too small
Less than 10 per cent of the originally planned 4,000 study participants ended up in the trial.
“Only 348 women were recruited – 174 in each arm – meaning that the trial was never going to have the statistical power, particularly when analysing potential harms,” said Levi.
Notably, study protocols indicate that Pfizer was given the green light as early as May 2021 by drug regulators to scale back the trial and reduce the sample size.
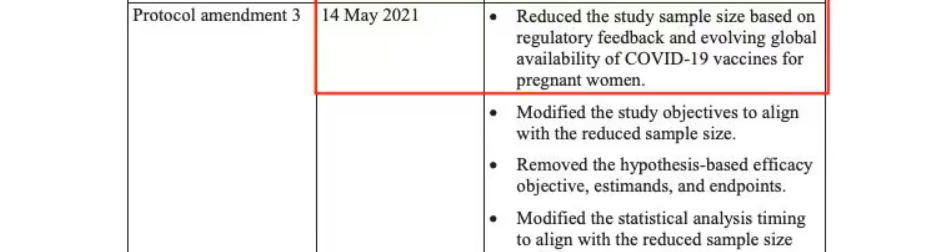
“To me, the wording in the protocol suggests that the FDA or another regulator basically gave Pfizer permission to do less,” remarked Levi.
“It’s not surprising though. The vaccine had already been recommended for pregnant women and many have taken it, so there is no upside to completing a trial that may detect signals of potential harms. It can only create problems for them, right?” he added.
Given that pregnant women were being vaccinated with a product that had not undergone rigorous safety testing in pregnancy, the FDA was asked if and why it allowed Pfizer to scale back the trial.
The FDA replied, “As a general matter, FDA does not comment on interactions it may or may not be having with sponsors about their clinical trials.”
Angela Spelsberg, an epidemiologist and medical director at the Comprehensive Cancer Center Aachen in Germany agreed that the integrity of the study had been compromised.
“There are just not enough babies in this trial to detect rare or very rare adverse events. We learned from studies in animals that lipid nanoparticles in the vaccine can deposit in many organs including the ovaries, so we must be extremely cautious about the potential negative impacts of the vaccine on reproductive health,” said Spelsberg.
“The scientific community urgently needs access to the pregnancy study data on the patient level for transparency and independent scrutiny of vaccine safety and efficacy because regulatory oversight is failing,” she added.
Exclusion criteria
The small sample size may have been the result of the strict selection process.
Pfizer recruited participants with an impeccable pregnancy history, and most were in their third trimester (27-34 weeks gestation), a stage when the baby’s major development had already occurred.
“It appears that they cherry picked the mothers to get the best results,” said Levi. “We have no idea what impact this vaccine has on the early stages of development of an embryo or foetus, because all the women had advanced pregnancies when they were recruited.”
Spelsberg agreed.
“The first trimester is particularly vulnerable to adverse reproductive health outcomes,” she said.
“Based on only weak observational evidence, regulators have reassured the public that the vaccines are safe throughout pregnancy. However, we don’t have reliable evidence on the vaccine’s impact on miscarriages, malformation, foetal deaths, and maternal health risks because they excluded pregnant women from pivotal trials,” added Spelsberg.
Missing data
Levi also noticed that “only partial data” were published.
“It doesn’t include any important metrics such as covid infections or antibody levels and its says we must wait until July 2024 for those results. It’s disturbing to say the least,” said Levi.
Also missing from the dataset was a full account of birth outcomes. Of the 348 women in the trial, Pfizer only reported on the birth of 335 live babies.
Of the 13 pregnancies unaccounted for, Pfizer reported one foetal death (stillbirth) in the vaccine group and the outcome of the other 12 pregnancies remains unknown.
“This is unacceptable,” said Levi. “Failing to report the outcome of 12 pregnancies could mask a potentially concerning signal of the vaccine in pregnancy. What happened to the babies, did they all die? Were their mothers vaccinated or unvaccinated?”
Trial dropouts
Finally, there were quite a few babies that were lost to follow-up in the trial.
“Twenty-nine babies in the placebo arm didn’t get to the end of the 6-month surveillance period, versus 15 babies in the vaccine arm. That’s almost double. Again, this is concerning and requires a detailed and transparent explanation,” said Levi.
Overall, both Levi and Spelsberg say the delays and failure to disclose vital data are unacceptable.
“Pfizer took a year to publish the data. When they finally did, it is incomplete. And we are expected to wait until July 2024 for the next batch of results, while authorities continue to recommend the vaccine in pregnant women,” said Levi.
“We still don’t have solid scientific evidence whether this vaccine is safe for pregnant women and their babies,” said Spelsberg. “It’s a tragedy and a scandal that vaccine use has been recommended, even mandated to women before, during and after pregnancy.”
Questions were put to Pfizer, but the company did not respond by the deadline.
Moderna is also conducting a clinical trial of its mRNA vaccine in pregnancy, but no data are available.
Reprinted from the author’s Substack









