Table of Contents
Penny Marie
Mum, woman, female. NZ-based independent investigative reporter, researcher, writer, coach, truth seeker. Founder of Let Kids Be Kids NZ.
A teenager in crisis, a fast‑tracked surgery
In 2019, 16‑year‑old female Fox Varian, then identifying as a ‘transgender boy’, sought help for intense psychological distress. She later told the court she was “desperate and terrified”, struggling with depression, anxiety, self‑harm and other serious mental‑health issues when she saw psychologist Dr Kenneth Einhorn.
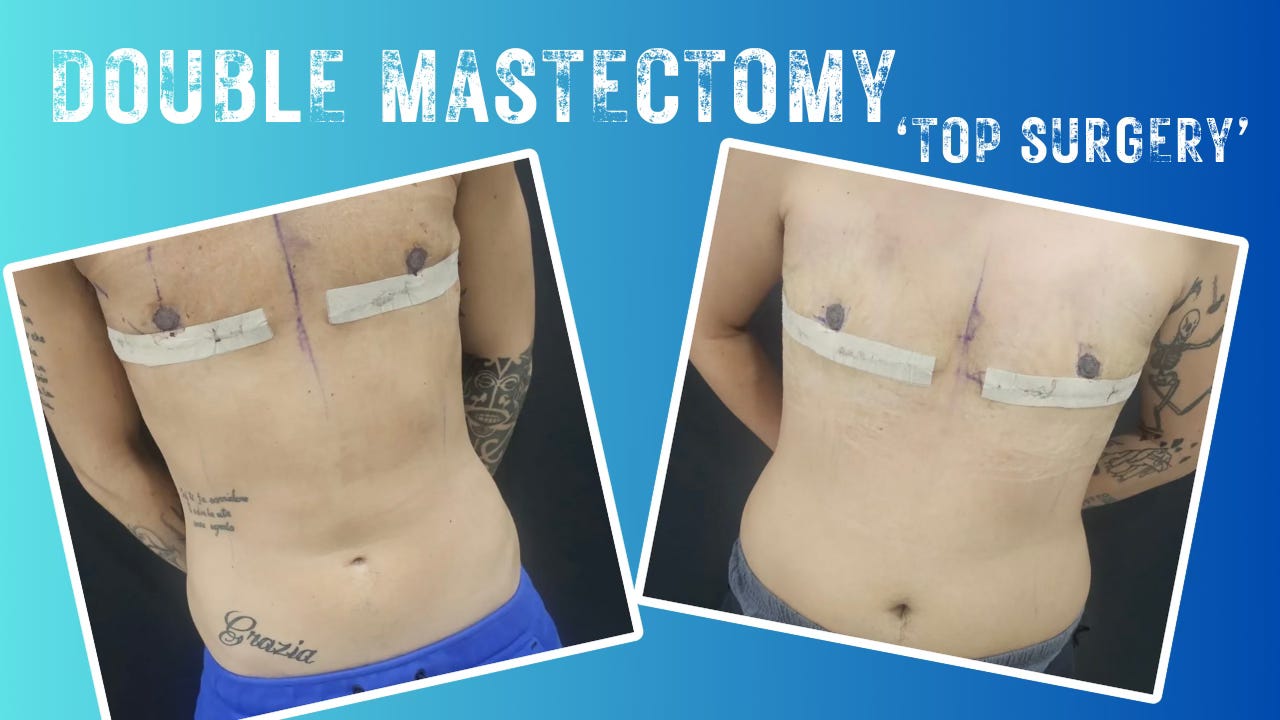
Instead of a slow, exploratory process, Varian says her care quickly narrowed to a single path: “top surgery” as the presumed solution to her distress. After a brief period under Einhorn’s care, he endorsed a double mastectomy for the teenager.
Plastic surgeon Dr Simon Chin then removed both healthy breasts, leaving permanent scars and loss of function that no later change of mind could reverse.
Varian would go on to detransition – that is – no longer identifying as male, and come to see the operation not as life‑saving medicine but as a grave error committed when she most needed robust mental‑health treatment.
Inside Varian v Einhorn: malpractice, not a culture‑war stunt
The lawsuit that followed was a conventional medical‑malpractice and personal‑injury case, not an abstract argument about identity. Filed in New York Supreme Court, Westchester County, it appears on the docket as Varian, Fox v Einhorn PhD, Kenneth et al., Index No. 61150/2023.
Varian sued:
- Psychologist Dr Kenneth Einhorn and Carmel Psychological Associates PC.
- Plastic surgeon Dr Simon Chin and his group, then part of CareMount Medical PC.
Her core claims were that Einhorn failed to meet professional standards in assessing a severely distressed minor before recommending irreversible surgery, and that Chin failed to obtain genuine informed consent or ensure that such drastic surgery was medically appropriate for a 16‑year‑old in crisis. She also alleged institutional failures in oversight and protocols at the practices that employed them.
In January 2026, after hearing expert testimony and Varian’s own account, a White Plains jury agreed. They found both doctors liable for malpractice and awarded her USD $2 million: USD $1.6 million for past and future pain and suffering, and USD $400,000 for future medical expenses, including treatment and potential reconstruction.
This was a public, contested trial that ended with a clear message: the way “gender‑affirming” principles were applied to this teenager fell below the standard of care the law requires.
When ‘affirmation’ replaces assessment
For years, leading US medical bodies have promoted “gender‑affirming care” as the preferred model for young people with gender distress. In practice, that has often meant treating a youth’s stated identity and stated goals – hormones, surgery, social transition – as the primary guide, while deeper exploration of trauma, psychiatric conditions or social pressures is sidelined.
Varian’s story exposes the risks of that approach. She describes arriving in profound distress and having that distress effectively reframed as proof that her body was the problem, and that amputation of healthy organs was the solution.
The legal question for jurors was not whether gender dysphoria is real, but whether competent clinicians can simply accept a vulnerable teen’s wish for radical surgery as decisive and then label it “care”.
Siding with Varian, the jury said no. Their verdict rejects the idea that “affirmation” can stand in for rigorous assessment, differential diagnosis and full disclosure of risks and uncertainties, especially when the patient is still a child.
The price of irreversibility – are ‘gender affirming’ institutions on notice?
At 16, Fox Varian had both of her healthy breasts removed. A double mastectomy, which the trans industry calls “top surgery”. At 22, she lives with scars, altered sensation, possible loss of breastfeeding, and a changed relationship to her own body that no change in identity can undo.
The jury’s choice to allocate most of the USD $2 million to pain and suffering rather than medical bills underscores that this loss was not treated as an unfortunate but acceptable side‑effect. It was treated as compensable harm caused by professional negligence.
This verdict matters well beyond one courtroom
New York is not a conservative jurisdiction, yet a jury there found a psychologist and a surgeon negligent while following a model widely marketed as ‘best practice’. By naming Carmel Psychological Associates and CareMount Medical alongside the individual doctors, the suit also puts larger clinics and corporate providers on notice that protocols which shortcut assessment or treat a teenager’s self‑diagnosis as decisive are not just ethically fraught, but legally dangerous.
For hospitals, universities and policymakers – including in countries like New Zealand, where these debates are often reduced to slogans – Varian v Einhorn offers a concrete narrative with legal weight:
- A distressed girl.
- A model of care that equated agreement with compassion.
- Clinicians and institutions that followed that script.
- And a jury that called it what the evidence showed in this case: not “affirming care”, but malpractice, with a very real price attached.
This article was originally published on by Let Kids Be Kids.









