Table of Contents
We will eventually beat COVID-19 using a vaccine and/or better health management and treatment, but until then we are reliant on information gleaned from data to control the spread and the severity of the disease. Unfortunately, the data collated to date is prompting more questions instead of answering them. For example, our COVID-19 data is not yet following overseas trends.
We don’t know if standard physical distancing of two metres is safe in all situations.
“A recent study at the University of Nebraska Medical Center that found widespread evidence of viral RNA in isolation rooms where patients with SARS-CoV-2 were receiving care” in air and surface samples. Even air collectors that were more than six feet away from patients detected the RNA, calling into question whether current social distancing guidelines are sufficient to prevent the spread of the disease.”
We don’t know exactly how the virus transmits. We know that direct contact such as sneezing on people and surfaces transmits the virus, but one study, yet to be peer reviewed, suspects that aerosols from medical procedures provide an airborne pathway.
“…surgical masks worn by sick patients reduced the detection of coronavirus RNA in both transmission forms, according to the NASEM report. Another preprint conducted in two Wuhan, China, hospitals indicates that staff movement, floor cleaning, and the removal of personal protective equipment could transmit the virus through the re-suspension of virus-contaminated aerosols.
“[I’m] relieved to see aerosolization is accepted,” says Kimberly Prather, an aerosol chemist at the University of California, San Diego, in remarks to Science. “This added airborne pathway helps explain why it is spreading so fast”.
The World Health Organization (WHO) states that airborne transmission may be possible during certain medical procedures such as intubation or open suctioning, but cautions that a recent study published in the New England Journal of Medicine that used a high-powered nebulizer to generate aerosols is not the same as real-life situations of people coughing.“
Further studies are needed to determine whether it is possible to detect COVID-19 virus in air samples from patient rooms where no procedures or support treatments that generate aerosols are ongoing.”
We don’t know why some people have very few symptoms or none, while others are severely affected and die.
The vast majority of confirmed cases are considered mild, involving mostly cold-like symptoms to mild pneumonia but 14% of confirmed cases are severe indicated by serious pneumonia and shortness of breath, another 5% develop respiratory failure, septic shock, and/or multi-organ failure and roughly 2.3% of confirmed cases resulted in death according to the latest and largest set of data on the new coronavirus outbreak released February 17 by the Chinese Center for Disease Control and Prevention.
It’s easy to understand why the elderly are more susceptible to severe COVID-19, but why do healthy young people die?
“It’s harder to explain why young, healthy people also sometimes die from the disease—for instance, Li Wenliang, a 34-year-old doctor who first sounded the alarm about the virus. He died a few weeks after contracting the pathogen.”
Overseas, why do more men than women die?
“It’s no secret that males are in many respects the frailer sex. On average, men die younger and are at more risk of life-threatening ailments, especially heart disease and many forms of cancer. The Sars-CoV-2 coronavirus seems to follow the same pattern. In all six of the countries that, up to 20 March, had sex-specific records of deaths from Covid-19, the proportion of men was higher than women. For four of those (China, France, Italy and South Korea), male mortality rates were more than 50% greater than female rates.
We don’t know why – but it doesn’t necessarily reflect differences in biology. Covid-19 is more dangerous for people with existing health issues, particularly cardiovascular or pulmonary (lung-obstructing) problems or hypertension – and these are all conditions that disproportionately affect men.”
Why is our COVID-19 age and gender distribution different from overseas?
Our gender and age grouping of COVID-19 cases here at 11 April does not follow overseas trends. Is this because we are in the early stages of the disease and our data trends will catch up with overseas trends over time? Are there other factors such as genetics in play?
“The trend was first seen in China, where one analysis found a fatality rate of 2.8% in men compared with 1.7% in women. Since then, the pattern has been mirrored in France, Germany, Iran, Italy, South Korea and Spain. In Italy, men have accounted for 71% of deaths and, in Spain, data released on Thursday suggests twice as many men as women have died.”
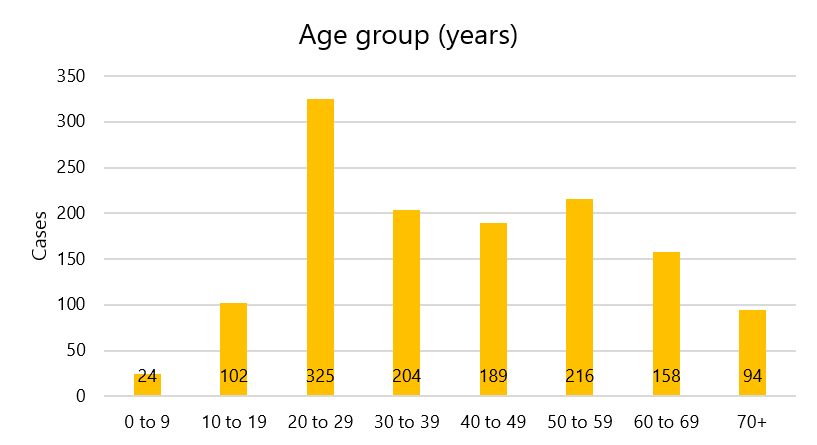
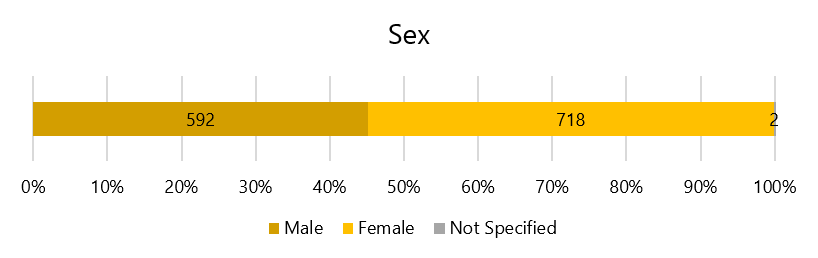
Graphs from NZ Health Department website from data compiled up to 11 April 2020.
If you enjoyed this BFD post please consider sharing it with your friends